Many adults—especially women—come to me with the same quiet question:
“Is this really ADHD… or is it trauma?”
They’re not asking out of curiosity.
They’re asking because they’ve tried productivity systems, medication, therapy, self-help—and still feel stuck, overwhelmed, or chronically dysregulated.
This question matters because ADHD and trauma can look strikingly similar on the surface, yet require very different kinds of support. And when we miss that distinction—or assume it has to be either/or—people often end up feeling worse, not better.
Let’s slow this down and look at what’s actually happening.
ADHD and Trauma: Why the Confusion Is So Common
ADHD is a neurodevelopmental condition that affects attention regulation, impulse control, working memory, and executive functioning.
Trauma, particularly chronic or developmental trauma, shapes the nervous system around safety and survival.
From the outside, both can present as:
- Difficulty focusing
- Disorganization and task paralysis
- Emotional reactivity
- Restlessness or shutdown
- Trouble following through
But the why underneath these behaviors is not the same.
That’s where things get missed.
Where ADHD and Trauma Overlap
ADHD and trauma often overlap in symptoms because both affect how the brain and nervous system process information.
Here’s a simplified way to think about it:
- ADHD struggles often stem from difficulty regulating attention and effort
- Trauma struggles often stem from difficulty regulating safety and arousal
When the nervous system doesn’t feel safe, focus naturally becomes harder.
When attention regulation is already challenging, stress hits harder.
This overlap is why misdiagnosis is common—and why many adults feel confused after receiving an ADHD diagnosis that doesn’t fully explain their experience.
Venn Diagram: Shared vs. Distinct Symptoms
The following Venn diagram illustrates the overlap and differences between ADHD and trauma-related symptoms.
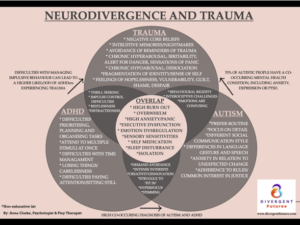
Shared symptoms may include:
- Inattention or “spacing out”
- Emotional overwhelm
- Difficulty with organization and planning
- Restlessness or agitation
More typical of trauma (not ADHD alone):
- Hypervigilance
- Intrusive thoughts or memories
- Avoidance behaviors
- Physiological stress symptoms (racing heart, nausea, muscle tension)
- Dissociation or emotional numbing
More typical of ADHD (not trauma alone):
- Chronic time blindness
- Excessive talking or interrupting
- Difficulty sustaining effort even in safe, calm environments
- Lifelong patterns present across many contexts
Venn diagram adapted from training materials by Anna Clarke, used here with attribution and permission.
One of the Most Important Questions to Ask
Instead of asking:
“What’s wrong with me?”
A more useful question is:
“Did these symptoms exist before stress and adversity—or did they intensify after?”
Here’s a general guideline clinicians use:
- ADHD symptoms tend to be consistent across environments and present early in life (diagnostically prior to age 12)
- Trauma-related symptoms often fluctuate with safety, stress, and relational context
This doesn’t mean it’s one or the other.
Many people—especially women with late diagnoses—have both ADHD and trauma, and the interaction between them can amplify symptoms in powerful ways.
Why “Safety First” Matters
One of the biggest mistakes I see is trying to treat attention challenges without first addressing nervous system regulation.
When someone’s system is in fight, flight, freeze, or shutdown:
- Focus tools don’t stick
- Productivity strategies feel impossible
- Medication alone may increase anxiety or agitation
This doesn’t mean ADHD medication is wrong.
It means regulation must come first.
A nervous system that doesn’t feel safe cannot sustain attention—no matter how motivated or capable someone is.
So… Is It ADHD, Trauma, or Both?
Often, the answer is both/and.
ADHD can increase vulnerability to trauma.
Trauma can intensify ADHD traits.
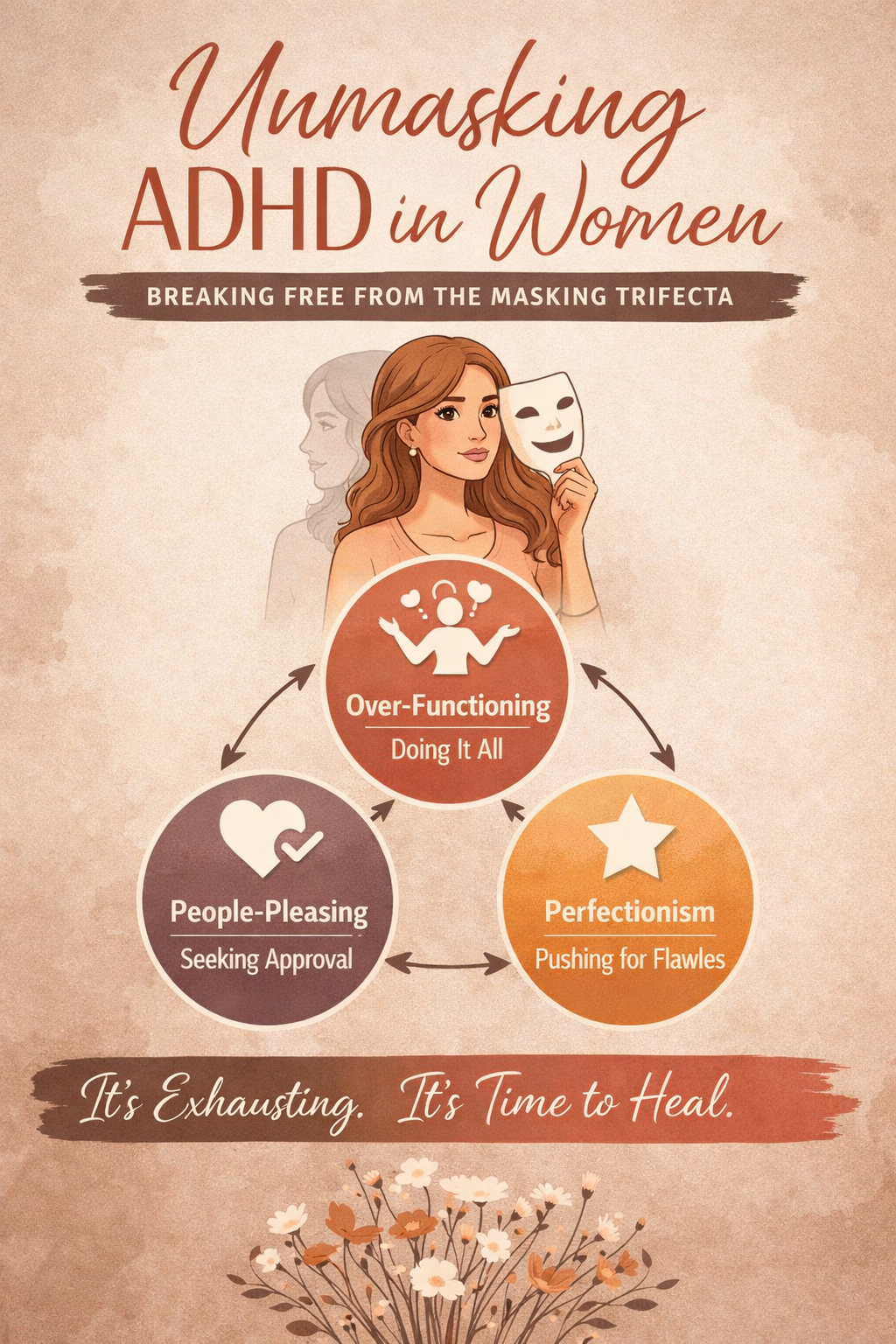
And chronic masking can blur the lines even further.
That’s why accurate assessment, nervous system awareness, and compassionate pacing matter so much—especially for high-functioning women who have spent years pushing through.
Want to Go Deeper?
If this topic resonates, I’ve explored it more fully in these two YouTube videos:
Is It ADHD or Trauma? Find Out Now!
The Hidden Trauma Behind ADHD
Both break this down in an accessible, nervous-system-informed way and may help you notice patterns you hadn’t seen before.
A Gentle Next Step
If you’re realizing that willpower, pressure, and “trying harder” haven’t worked—and you’re craving a more compassionate, body-aware approach—
✨ The Self-Loved ADHD Woman Way: How to Stop Playing Small with ADHD is a guided journal-book experience designed to help you slow down, regulate your nervous system, and reconnect with yourself without fixing or forcing.
It’s not about labels.
It’s about learning how your system works—and meeting it with care.
You can learn more here:
👉 https://jenbarnes.org/stop-playing-small/